- HOME
- Digital Health
- How wearable technology is transforming preventive healthcare
How wearable technology is transforming preventive healthcare
- Last Updated : August 1, 2025
- 295 Views
- 13 Min Read

What if I told you that a tiny device on your skin could warn you of a heart attack days before you feel a twinge? Or keep your diabetes in check without pricking your fingers with a needle every single day?
That's the power of wearable technology, and it's transforming preventive healthcare into something personal, proactive, and life-changing. The result? Over the next 25 years, wearable technology will deliver global healthcare cost savings of about $200 billion, primarily due to improved disease prediction and early intervention capabilities.
With chronic conditions like diabetes and heart diseases on the rise, these devices are spotting risks early, keeping us healthier, and making wellness feel like a superpower. In this blog post, let's dive into how wearable technology can prove to be an important factor in preventive healthcare in the future and beyond.
The wearable tech boom
Imagine a health coach that's always on, tracking your vitals and nudging you to make smarter choices. That's wearable tech; think fitness trackers, smart fabrics, biosensors, and even brain-computer interfaces that sound like sci-fi but are real.
The wearable market is racing toward $151.8 billion by 2029, growing at a blazing 27.5% annually. Why? Because with 1.28 billion people managing hypertension and 537 million tackling diabetes, we need tools to outsmart these conditions.
Wearable devices are impressively accurate for monitoring vital signs like heart rate. Studies show mean errors under 5% at rest and temperature readings with median absolute percentage errors as low as 1.7%. These devices are evolving fast from wristbands to neural implants; wearables are making prevention proactive, not reactive.
10 wearable devices reshaping preventive healthcare
From everyday gadgets to futuristic prototypes, these ten devices showcase the depth of wearable tech. We'll break down how each one works, what makes it stand out, how it's improved over earlier versions, and how it empowers preventive healthcare.
1. Continuous glucose monitors
Continuous glucose monitors (CGMs) are a lifeline for the 589 million adults living with diabetes worldwide. These small, discreet sensors are inserted just under the skin and measure glucose in interstitial fluid every few minutes using an enzyme-based electrochemical reaction.
Modern CGMs, like the Dexcom G7, are about 60% smaller than previous models and require only a 30-minute warm-up, compared to two hours for older devices. These devices transmit glucose data wirelessly to smartphones or receivers, and advanced systems provide predictive alerts for high or low glucose levels up to 20 minutes in advance. Many CGMs now integrate with compatible insulin pumps, enabling automated insulin delivery for better glucose management.
GCMs achieve a mean absolute relative difference of 8.2% in adults, reflecting high accuracy compared to earlier models. Improved accuracy at low glucose levels helps prevent dangerous hypoglycemia. Recent studies show that regular use of CGMs can reduce HbA1c by about 0.5%, which lowers the risk of complications such as neuropathy and kidney failure, and reduces hospital visits.
It also enables early intervention by alerting users to glucose trends before they become critical, reducing the risk of diabetic emergencies and long-term organ damage through timely diet or insulin adjustments.
2. Heart rate monitors
Heart rate monitors—commonly found in smartwatches like the Apple Watch and Fitbit Versa—use photoplethysmography (PPG), where green LED lights track changes in blood flow at the wrist to measure heart rate.
Recent reviews and tests show that these devices are accurate in measuring heart rate, with correlation coefficients typically ranging from 0.93 to 0.99 compared to reference ECG devices (depending on activity and model). Some models also include electrical sensors to provide electrocardiogram (ECG) readings, which can detect atrial fibrillation (AFib), a condition affecting more than 33 million people worldwide.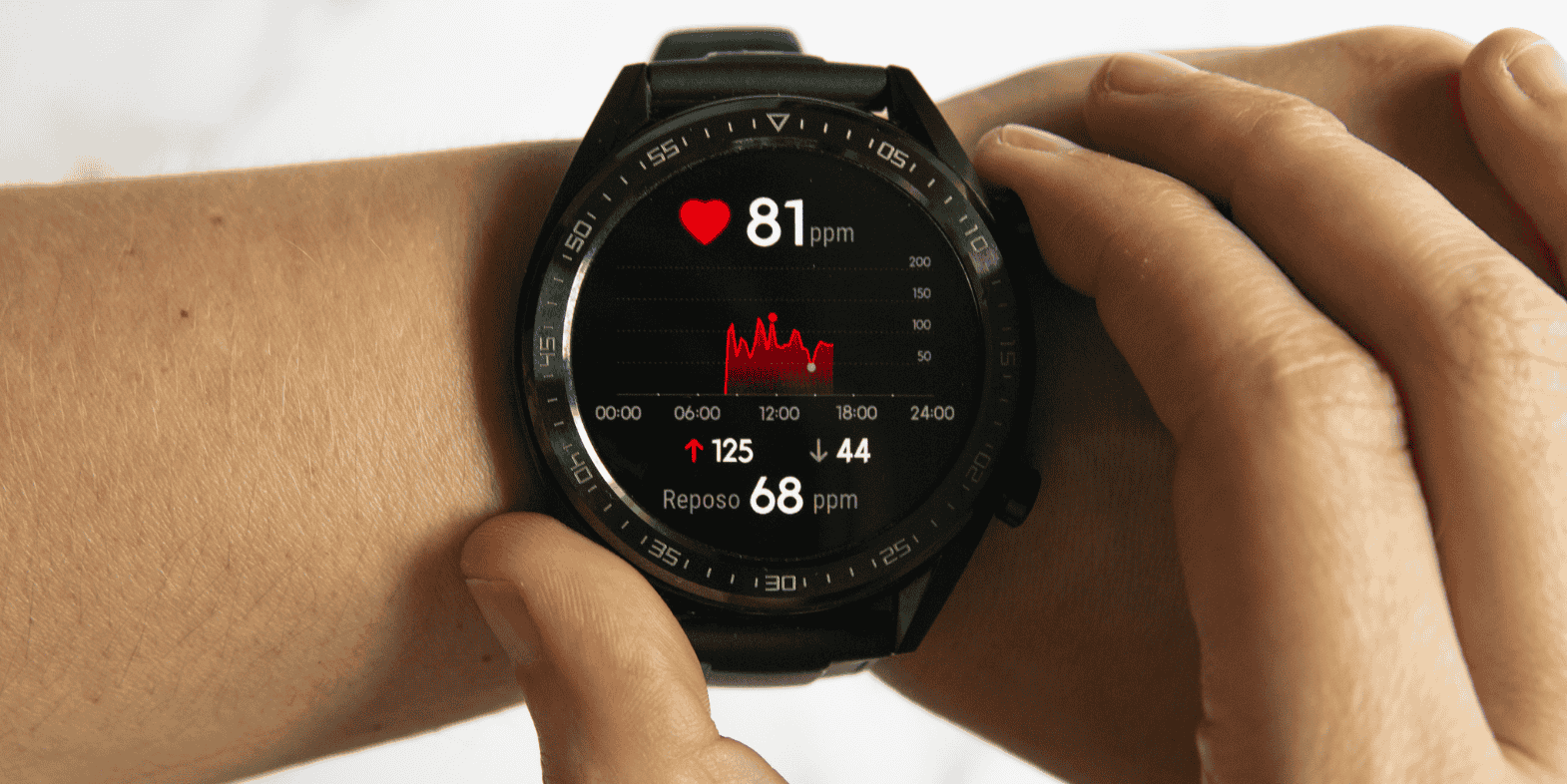
Newer smartwatches offer additional features, such as blood oxygen (SpO2) monitoring and faster processors for more seamless data analysis, compared to earlier generations that often lacked ECG capability or had shorter battery life. A landmark 2024 Norwegian study of post-surgery patients found the Apple Watch ECG detected atrial fibrillation with 91% sensitivity and 96% specificity, closely matching clinical monitors
By detecting AFib or stress through heart rate variability (HRV), these devices support early intervention, potentially preventing strokes and encouraging healthy habits like meditation. Early detection of abnormal rhythms enables timely medical care to reduce the risk of stroke or heart failure, while HRV insights help users manage stress and lower cardiovascular risk.
3. Body temperature monitors
Body temperature monitors, such as those in smart rings and wearable patches, use infrared sensors to measure skin temperature continuously—often every minute—detecting deviations from your personal baseline. Large-scale studies have shown that these wearables, when combining temperature with other physiological signals like heart rate and respiratory rate, can detect signs of illness, including COVID-19, an average of 2.75 days before users seek diagnostic testing.
By combining temperature, heart rate, and movement data, these wearables can assess illness risk and, for women, help track ovulation cycles by syncing data to an app.
Compared to earlier versions, modern devices are slimmer, include blood oxygen tracking, and leverage AI to predict illness up to three days before symptoms appear.
Early fever detection helps prevent the spread of infectious diseases, while fertility insights enable proactive reproductive health management. In preventive healthcare, these monitors allow for early intervention, reducing disease progression and complications, and supporting informed family planning decisions.
4. Pulse oximeters
Pulse oximeters integrated into wearable devices use red and infrared LEDs to measure blood oxygen saturation by analyzing light absorption differences in the blood. Clinical validation studies have shown that wrist-worn pulse oximeters can achieve strong correlation with clinical-grade reference devices, with correlation coefficients typically in the range of 0.94 to 0.95, with a mean bias of about 1% and a root mean square error (RMSE) of approximately 3%.
Average blood oxygen readings from these wearables closely match those from medical-grade devices, though measurement success rates can vary, with some studies reporting about 69.5% of attempted readings yielding usable data, as detailed in a peer-reviewed clinical study.
These devices monitor SpO2 during sleep and physical activity, and newer models often include features such as ECG recording and sleep apnea detection, along with extended battery life compared to earlier fitness trackers.
During the COVID-19 pandemic, pulse oximeters played a critical role in the early detection of “silent hypoxia,” which enabled timely medical intervention and contributed to reduced mortality, though the exact impact on death rates varies by population and study. For individuals with chronic respiratory conditions such as COPD or sleep apnea, regular SpO2 monitoring helps prevent respiratory failure by alerting users and clinicians to low oxygen levels, supporting timely intervention.
5. Sleep trackers
Sleep trackers integrated into wearable devices use a combination of accelerometers, photoplethysmography (PPG) sensors, and heart rate variability analysis to estimate sleep duration, sleep efficiency, and sleep stages such as light, deep, and REM sleep.
Large-scale studies have shown over 90% agreement and sensitivity compared to polysomnography, the clinical gold standard, validating these technologies for high accuracy in detecting total sleep time and sleep-wake periods. Recent validation studies report sensitivity ranging from 50% to 86% for distinguishing specific sleep stages, depending on the device and the particular sleep stage being measured.
Modern sleep trackers often include additional features, such as blood oxygen and skin temperature monitoring, as well as advanced algorithms that provide personalized sleep insights and recommendations. These improvements enable more comprehensive assessments of sleep quality and recovery, helping users optimize their rest habits.
Insufficient sleep is strongly associated with increased health risks. Epidemiological research shows that poor sleep can raise the risk of cardiovascular disease by up to 48% and stroke by 15%. By providing actionable feedback on sleep patterns, wearable sleep trackers support preventive healthcare, helping users identify and address poor sleep habits, which in turn can reduce the risk of chronic diseases and improve overall well-being.
6. Smart clothing
Smart clothing integrates textile-based sensors to monitor physiological metrics, such as heart rate, respiratory rate, and movement. These sensors, made of woven electrodes and embedded accelerometers, enable continuous, real-time tracking of vital signs, including ECG-like signals and respiration patterns. Recent advancements have made these garments significantly lighter, more breathable, and more comfortable, addressing earlier challenges of bulkiness and limited washability.
Accuracy for specific applications, such as sleep state detection, has reached up to 98.6% in laboratory settings using AI algorithms applied to smart textiles. Smart clothing has been validated for reliable measurement of heart rate and respiration, supporting early detection of health changes and chronic disease management for cardio-respiratory monitoring. Modern smart textiles can also transmit data wirelessly to cloud-based platforms and integrate with electronic health records (EHR), expanding their use in remote monitoring and telemedicine.
The technology is advancing rapidly, with the global smart textile market projected to grow from $22.08 billion in 2025 to over $274.99 billion by 2034, driven by demand for health monitoring and activity tracking. In preventive healthcare, continuous monitoring of cardio-respiratory parameters can help detect early signs of asthma exacerbations or heart failure, supporting timely intervention and personalized exercise regimens to reduce cardiovascular risk.
7. Stress monitors
Stress monitors integrated into wearable devices use physiological signals such as heart rate variability, electrodermal activity (EDA), and, in some advanced systems, sweat-based cortisol to detect and predict stress episodes.
Machine learning models trained on these biosignals have demonstrated a pooled mean accuracy of approximately 85.6% for stress detection. Some machine learning approaches, especially those combining EDA and heart rate data, have achieved even higher classification accuracy up to 95% with algorithms like linear discriminant analysis, support vector machines, and fuzzy logic.
Modern stress monitors often feature longer battery life, real-time data syncing, and advanced analytics for personalized coping recommendations. Unlike earlier vibration-based or single-sensor devices, current wearables provide multi-sensor, clinical-grade data, and some are being validated for additional applications such as seizure or epilepsy monitoring.
By providing early detection and actionable feedback, wearable stress monitors can help prevent anxiety-driven health issues like hypertension and support interventions that foster mental well-being and reduce chronic disease risk.
8. Blood pressure monitors
Wearable blood pressure monitors, especially the latest chest patches, can check your blood pressure automatically every 15 minutes throughout the day. These devices are highly accurate, with about 95% of their readings matching standard medical equipment. The results are sent wirelessly to secure cloud platforms, so your healthcare provider can review your blood pressure trends in real time and make timely recommendations if needed.
Recent developments in wearable blood pressure technology have resulted in patches that are about 30% smaller and more adhesive-friendly, while also integrating heart rate variability (HRV) analysis for additional stress and cardiovascular insights. These improvements enhance the detection of masked hypertension and provide more reliable continuous monitoring compared to earlier or cuff-based devices.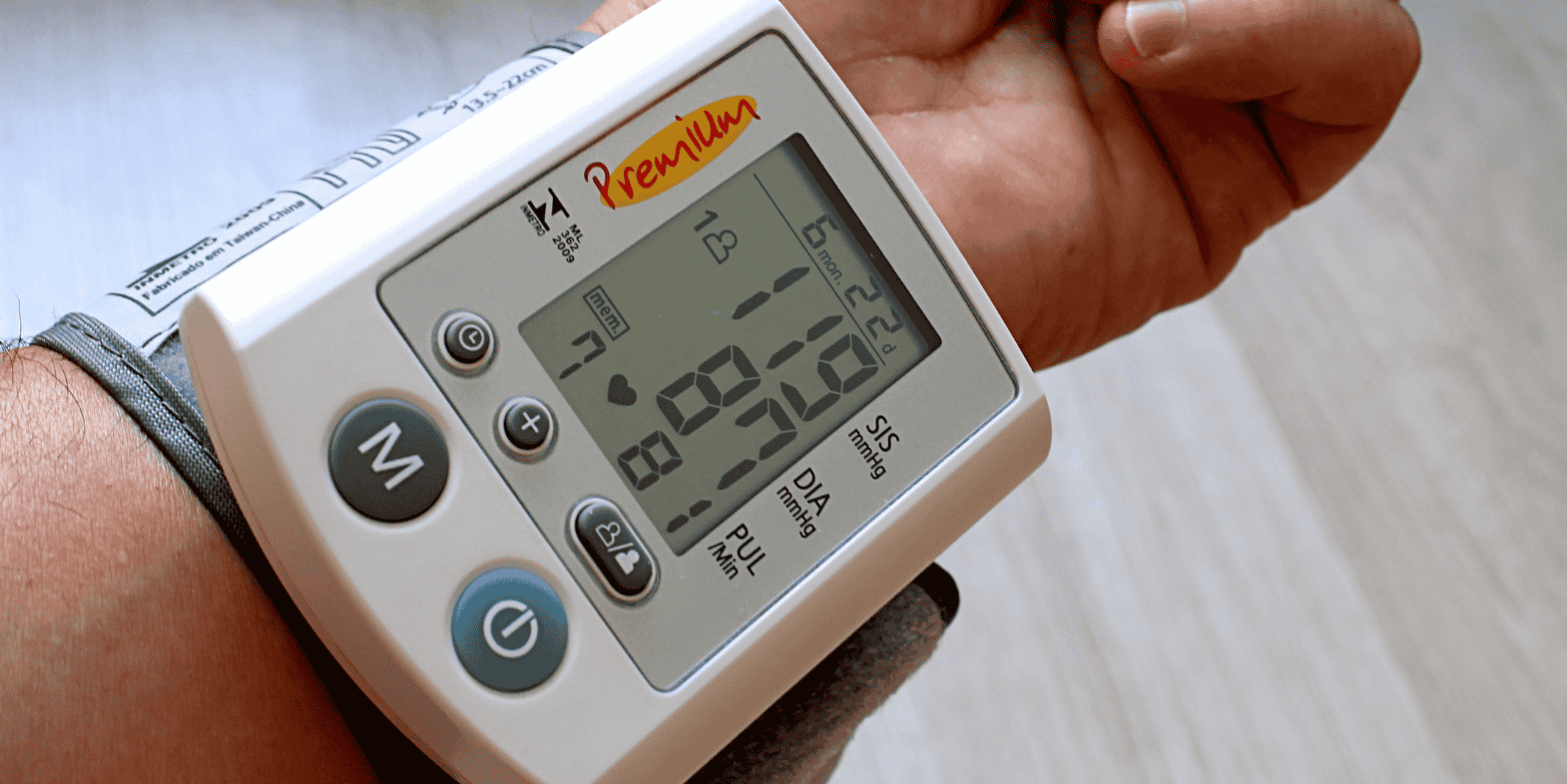
Hypertension remains a significant public health concern, affecting about 45% of adults in the United States, according to the Centers for Disease Control and Prevention. Continuous blood pressure monitoring helps prevent serious events like strokes and heart attacks by flagging anomalies early, empowering individuals and healthcare providers to make timely adjustments to diet, medication, or lifestyle.
In preventive healthcare, ongoing blood pressure tracking enables early identification of abnormal trends, supporting interventions that reduce cardiovascular risk and improve long-term health outcomes.
9. Wearable ultrasound patches
Wearable ultrasound patches are an emerging technology that use flexible, stretchable piezoelectric transducers to generate sound waves and produce real-time images of internal organs, such as the heart.
Recent research demonstrates that these patches can provide blood pressure and cardiac monitoring results that closely match those of standard clinical devices, enabling reliable, continuous assessment from home. Designed as comfortable adhesive patches, they wirelessly transmit data to clinicians for remote evaluation, offering a portable and user-friendly alternative to traditional, bulky ultrasound machines.
These advances are particularly valuable for patients with heart disease. Wearable ultrasound can catch cardiac abnormalities early and help prevent heart failure by enabling timely medical intervention. In prenatal care, continuous at-home monitoring with these patches can support healthier pregnancies by detecting fetal issues sooner and reducing the need for frequent clinic visits.
By making high-quality imaging accessible outside of clinical settings, wearable ultrasound patches have the potential to transform preventive healthcare, enabling early detection of cardiac or pregnancy complications and supporting prompt, effective treatment.
10. Neuralink brain-computer interface
Neuralink, a brain-computer interface, consists of a coin-sized implant embedded into the brain with over 1,000 ultra-thin electrodes that read neural signals. These electrodes are inserted into the motor cortex using a specialized surgical robot, enabling precise recording of individual neuron activity.
The implant processes these signals and transmits them wirelessly via Bluetooth to external devices, which can be worn as headsets or connected to computers, allowing users to control digital interfaces with their thoughts. In 2024, Neuralink conducted a human trial where a quadriplegic participant successfully controlled a computer cursor using the implant, marking a significant milestone in brain–machine communication.
Unlike earlier brain–computer interfaces that relied on wired connections, Neuralink’s wireless design offers enhanced precision and user mobility. Although still awaiting full regulatory approval, the technology holds promise for monitoring brain activity in neurological conditions, such as epilepsy and Parkinson’s disease, which affect approximately 50 million and 10 million people worldwide, respectively, according to the World Health Organization. By detecting seizure patterns or motor dysfunction early, Neuralink may help prevent neurological crises and improve disease management.
Neuralink’s real-time brain monitoring capabilities may enable early interventions to manage epilepsy or slow Parkinson’s progression, potentially reducing the frequency and severity of neurological emergencies and enhancing quality of life.
Wearable tech becoming your personal health assistant
Wearable technology is quietly transforming how we care for ourselves, making health management more proactive, personal, and connected than ever before. They’re quietly becoming an essential part of everyday health, empowering you to take charge and stay connected to your care team anytime, anywhere.
24/7 health tracking
Gone are the days when you had to wait for an annual check-up to know how you’re doing. Today’s wearables can monitor everything from your heart rate to your blood sugar, and even brain signals, all in real time. This gives both you and your healthcare provider a clearer, more continuous picture of your well-being.
Early risk detection
With the help of artificial intelligence, wearables can alert you to potential health issues before they become serious. Whether it’s catching heart irregularities with an ultrasound patch or spotting early signs of a neurological event, these devices help you stay one step ahead and avoid unnecessary trips to the hospital.
Personalized health nudges
Wearables don’t just track your stats; they also encourage better habits. From gentle reminders to move more, to prompts for better sleep or stress management, these personalized nudges help you build routines that support long-term health.
Remote doctor connection
Remote patient monitoring means your vital signs can be shared securely with your doctor, no matter where you are. This makes healthcare more accessible, especially for those managing chronic conditions or living far from medical centers, and helps keep you connected to care when you need it most.
Challenges holding wearables back
While wearable tech is making big strides in health and wellness, it still faces some real hurdles. It has immense promise, but overcoming these challenges is key to making it work for everyone.
Data privacy concerns
Wearables collect deeply personal health information—like your heart rate, sleep patterns, or even brain activity. If this data isn’t protected, there’s a risk it could be accessed by hackers or misused by companies. For many, trusting these devices means knowing their private health data is safe and secure.
One size doesn’t fit all
Not everyone’s body works the same way, but many wearables use algorithms built for the “average” person. This can lead to readings that aren’t as accurate for people with different skin tones, unique health conditions, or unusual sleep cycles. Until these devices become more personalized, some users may not get the full benefits.
Unequal access
Wearables can be pricey and sometimes tricky to use, which puts them out of reach for many older adults and families on tight budgets. This means the health advantages of these devices aren’t available to everyone, potentially widening health gaps.
Users giving up too soon
It’s not uncommon for people to buy a wearable, get excited for a week, and then leave it in a drawer. Complicated apps, uncomfortable bands, or unclear instructions can make people give up quickly, especially if they’re not tech-savvy. Making devices simpler and more comfortable can help more people stick with them.
Integration with healthcare systems
Even if your wearable tracks your health perfectly, it doesn’t always play nicely with your doctor’s systems. If your health data can’t be easily shared with your care team, it’s less useful for managing your health. Better integration with healthcare systems would help wearables reach their full potential in supporting your well-being.
What’s next for wearable health tech
Despite these challenges, the future of wearable tech is bursting with potential. For those just dipping their toes into this area, here’s what’s coming down the pipeline and why it’s so exciting.
Smarter AI predictions
Artificial intelligence is rapidly making wearables more intuitive and insightful. Soon, your device won’t just track your health; it will learn your unique patterns and offer personalized warnings or advice, helping you act before small issues become big problems.
Health in your clothes
Wearables are blending seamlessly into everyday life. Imagine putting on a shirt or jacket that quietly tracks your heart rate, breathing, or stress levels as you go about your day. These smart textiles are designed to be comfortable, washable, and as easy to wear as any regular clothing, making health monitoring effortless.
Brain-boosting tech
The next wave of wearables is pushing into new territory, like brain–computer interfaces. These devices may one day help spot early signs of neurological conditions or mental health changes, giving people and doctors a head start in managing brain health. As this technology evolves, it might work alongside more familiar wearables, making brain health as trackable as your daily steps.
Making wearables for everyone
The goal is to make wearables accessible to all, not just the tech-savvy or those with deep pockets. Designers are working on simpler, more affordable devices and easy-to-use apps so that everyone, including older adults and people in underserved communities, can benefit from these advances.
The bottom line
Wearable technology is quickly becoming a game-changer for personal health. From glucose monitors that help manage diabetes to brain interfaces that could one day monitor your mental well-being, these devices are making it easier than ever to keep tabs on your health. They track your vital signs around the clock, catch risks early, encourage smarter habits, and keep you connected to your care team—all from the comfort of home.
While there’s still work to do around privacy and making these tools accessible for everyone, the future looks bright. With advances in AI, smart fabrics, and even brain tech on the horizon, taking charge of your health is becoming more seamless and empowering. Whether you’re slipping on a fitness tracker or simply dreaming about what’s next, your journey to better health can start today.